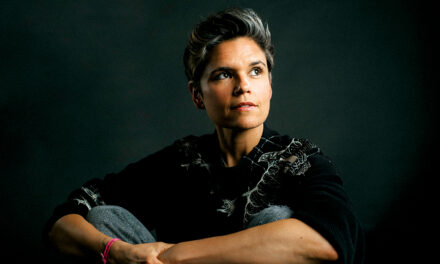
As director of thoracic surgery for Capital Health, Africa F. Wallace, MD, is dedicated to making a lasting impact on every patient she sees and a meaningful change to lung cancer survival rates.
or Africa F. Wallace, MD, her childhood dream of becoming a doctor wasn’t like playing dress-up or make-believe. It was the ignition of a plan, fostered by her parents’ encouragement of her aptitude and interest in science and math and fueled by her own family doctor, an inspiring physician who left a “lasting impression.”
Dr. Wallace was methodical and singularly focused in her pursuit of that goal, plowing through her Bachelor of Arts in biology at Harvard University and her medical degree from the Georgetown University School of Medicine in Washington, DC. She completed her general surgery residency at Georgetown University Hospital and her cardiothoracic surgery residency at the University of Pittsburgh Medical Center. After her first year of med school, Dr. Wallace knew she wanted to become a surgeon, and she homed in on cardiothoracic surgery, which focuses on surgical procedures on organs injured in the chest. “Throughout medical school, [internships, and residencies], you learn to deal with disease processes. You learn all the logistics that go into being in medicine, even the parts that sometimes don’t feel as fulfilling (like paperwork),” she says. “However, with time, I’ve gained absolute clarity and a profound understanding of my ultimate responsibility in the realm of medicine.”
In her role as Director of Thoracic Surgery at Capital Health, Dr. Wallace performs procedures to treat cancer and other serious conditions, so that responsibility is her North Star. “I used to think my primary job as a surgeon was to effectively treat thoracic disease processes and remove cancer through surgery. However, beyond the technical aspects of my profession, my greater mission is to be a source of inspiration for my patients, especially those battling cancer,” she says. “In the midst of despair, I aim to offer not just a medical solution but to be a beacon of hope, striving to uplift patients during their challenging journey toward recovery.”
There’s one patient in particular who is never too far from Dr. Wallace’s mind—an otherwise healthy, vibrant, career-oriented woman who ended up in her office at Capital Health – Hopewell with locally advanced lung cancer. She needed chemotherapy and radiation before Dr. Wallace could perform surgery, and based on the location of the cancer, some disfiguration and partial loss
of function was possible. Initially the patient resisted surgical treatment.
After her chemotherapy and radiation, the patient came back to Dr. Wallace with a new outlook. “She just looked at me and said, ‘Dr. Wallace, I trust you.’ I was able to get the cancer out without disfiguring her chest wall or injuring any nerves that might have affected her arm. Now she and her husband are like family to us,” she explains. “I understand that patients are putting their lives in my hands. I’m asking you to trust me to take you to a place you’ve never been to do something that’s never been done to you before that comes with significant risks. My goal is to instill the confidence that I’m going to keep you safe.”
I used to think my primary job as a surgeon was to effectively treat thoracic disease processes and remove cancer through surgery. However, beyond the technical aspects of my profession, my greater mission is to be a source of inspiration for my patients, especially those battling cancer.

I see a higher calling for myself, and I don’t know
if that’s in hospital administration or some form of policymaking, but
I know I can be part of positive change.

No "I" in Team
As a key member of Capital Health’s Lung Center of Excellence, Capital Health Surgical Group, and Capital Health’s Robotic Center of Excellence, Dr. Wallace knows she could not perform at the highest level without the very best team of medical professionals (in and out of the operating room) around her. Her colleagues also believe, like she does, in a vision of a better delivery of lung cancer treatment, and they are dedicated to making it happen.
“We share a common goal of making a meaningful difference and enhancing outcomes for our patients. What I’ve found to be my unique strength, my superpower, is not only connecting with my patients but also fostering genuine connections with my colleagues. It goes beyond mere directives; it’s about truly understanding them, caring for them, and collaborating effectively. I feel honored and blessed to have such a dedicated team by my side.”
Advances in Treatment
Among other specialties, Dr. Wallace is a master at performing minimally invasive procedures to remove lung cancer, esophageal cancer, and tumors of the mediastinum (the area of the chest that separates the lungs). She also treats benign conditions of the thoracic cavity and esophagus. Among the many advances in diagnostics and treatment, Capital Health is the first hospital in Mercer County, NJ, to offer a robotic-assisted lung biopsy technology that Dr. Wallace says is a game changer. “This robotic platform extends the capabilities of lung biopsy technology, surpassing the limitations of standard diagnostic tools that were once the primary option,” she explains. “By leveraging this advanced system, we can now access areas previously deemed unreachable, providing a more comprehensive and precise approach to diagnosis. This represents a significant leap forward in our ability to improve diagnostic accuracy and patient outcomes in the realm of lung biopsies.”
The robotic-assisted procedures using the da Vinci surgical system enable Dr. Wallace to visualize the inside of a patient’s body with a high-definition 3D camera to perform complex procedures with minimal invasiveness and reduced recovery time. The improvements in technology and medication are giving doctors a greater arsenal with which to fight cancer, and it’s making a significant difference. Since Dr. Wallace took her post at Capital Health in 2019, there have been modest improvements in national lung cancer survival rates.
However, Dr. Wallace says there is still a long way to go—lung cancer is still the leading cause of cancer deaths. In the United States, lung cancer accounts for about 20 percent of all cancer deaths, which is more than that of breast, colon, and prostate cancers combined. “We’ve achieved notable strides in the treatment of lung cancer. Four years ago, the collective 5-year survival rate for all stages I through IV stood at 15 percent. I’m encouraged to report that it has risen to 21 percent. While this marks significant progress, a 21 percent survival rate falls short of winning the war against lung cancer. Especially when compared with other cancers, such as breast cancer, which has a 91 percent 5-year survival rate for all stages combined.” Dr. Wallace says. “At present, there is an average of 86 days from the detection of lung cancer to the initiation of treatment. Despite the emergence of new medications and advancements in surgical techniques, there’s still so much work to be done.”
A Surgeon With a Vision
Last November, Dr. Wallace was named president of the Eastern Cardiothoracic Surgical Society (ECTSS), which was the first time in the organization’s 60-year history that a Black woman has ascended to that post. It was so notable, in fact, both Essence and Black Enterprise published articles online to recognize the event.
She also serves on the Diversity, Equity, and Inclusion Work Force of the Society of Thoracic Surgery and is a member of the Women in Thoracic Surgery and Association of Women Surgeons. With all that access to information supplementing what she sees at the hospital each day, Dr. Wallace is building toward something—a desire to make a powerful and lasting impact on the access to information and treatment of lung cancer. “I don’t think my work will continue to be solely in the operating room. I have an opportunity to have a broader impact on the delivery of lung cancer care from start to finish, and that includes how we provide access to patients who typically would not have it,” Dr. Wallace explains.
For example, she wants to disseminate health education to the public at large, with a specific emphasis on underserved minorities and people in lower socioeconomic communities. According to the Centers for Disease Control and Prevention (CDC), smoking cigarettes causes between 80 percent to 90 percent of lung cancer deaths. The CDC also reports that people with lower incomes have higher incidence of commercial tobacco-related diseases than people with higher levels of income.
Dr. Wallace wants to be part of the solution to ensure that patients who typically don’t receive the message that smoking is detrimental to health not only receive it but have ready access to screenings and diagnostics. “My focus now extends beyond medications and surgery. The call to improve the accessibility and efficiency of our processes is urgent and apparent. I am increasingly recognizing the need to build comprehensive systems where patients, armed with understanding, can take meaningful actions,” Dr. Wallace says. “I see a higher calling for myself, and I don’t know if that’s in hospital administration or some form of policymaking, but I know I can be part of positive change.”