Last October, on one of her walks with her dog, Emmett, 76-year-old Eileen Aviss felt tightness in her chest. She went home and Googled the symptoms to try to figure out what was going on in her bod, but the feeling went away, and she let. But on another walk—one of the hilly ones—she felt the tightness again, but this time she also felt nauseous. “My husband, John, looked over with concern and said, ‘Do you think you’re having a heart attack?’” she recalls.
With a sense of worry and dread, Aviss made an appointment with her doctor at Capital Health, Shaismy Kudakachira, DO, who thought it sounded serious enough to connect her to a cardiologist for a series of tests. The doctor ordered an electrocardiogram (EKG) to measure the electrical efficiency of her heart, which was inconclusive. That was followed by an echocardiogram (echo), an ultrasound of the heart, which didn’t show anything ominous. But then the doctor performed a nuclear stress test, which uses a small amount of radioactive material (tracer) and an imaging machine to show blood flow to your heart while you exercise. That’s when the doctor could see three blocked arteries. Without intervention, they told Aviss, she could have a heart attack.
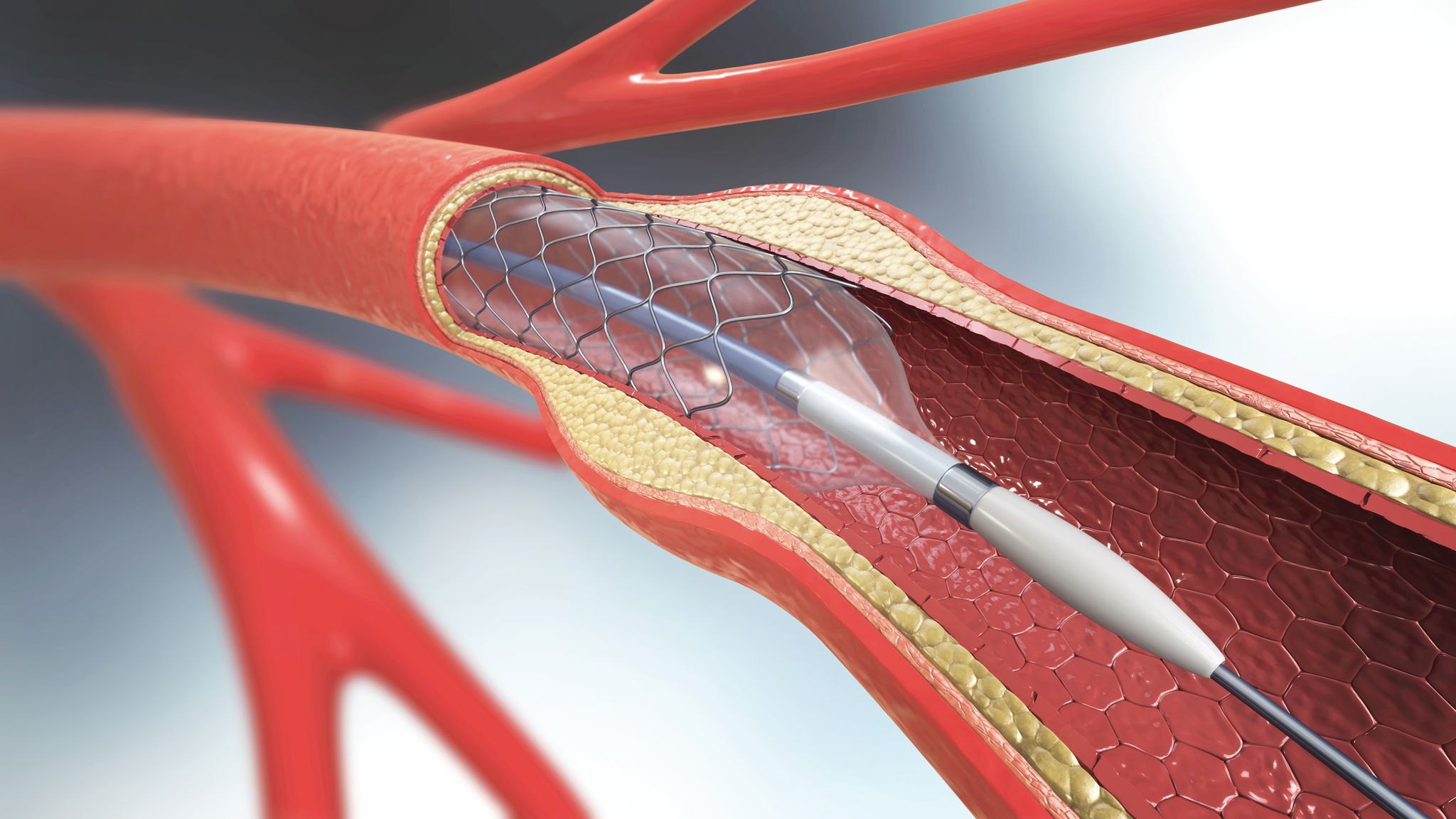
Doctors wanted to do a procedure called a coronary angioplasty with stenting, in which a tiny balloon catheter is inserted into a blocked blood vessel to help widen it and improve blood flow to the heart. Prior to angioplasty, open-heart bypass surgery was the main option for patients Angioplasty—especially the refined version available at Capital Health today—offers a much faster recovery time since it’s non-invasive.
First introduced in 1974, balloon angioplasty with stenting has become the most frequently used treatment in vascular emergencies of the heart. However, to help patients avoid cardiac emergencies, Capital Health endeavored to offer elective coronary angioplasty for more than a decade. The good news for Aviss was that Capital Health was approved last February, which meant she didn’t have to wait to schedule the procedure and could have it all done by the time she and her husband, John, planned to head to Florida this February.“
To gain approval, hospitals have to demonstrate that they can do emergency coronary angioplasty and stent placement safely, and we did that,” says Harit Desai, MD, director of the cardiac catherization lab at Capital Health.