Too many of us can’t sleep, and it’s impacting our mental and physical health in more ways than most of us know. Here’s how much sleep you need, why you need it, and a prescription for what to do when you find yourself tired, out of sync, and wide awake.
It feels like everyone in the whole world is asleep except me. It’s 3 o’clock in the morning, and I’m wide awake. My mind is ping-ponging between mulling over my day to worrying about the bills to thinking about my boys to stressing over my Real Woman deadline. So I lie in bed and watch the electronic digits light up the clock across the room, counting off the seconds, minutes, and hours I’ll never get back. I try clearing my mind. I try listening to a podcast. Nothing works—I still can’t fall asleep.
But I have plenty of company. A report released last year by the Centers for Disease Control and Prevention (CDC) found lack of sleep to be a public health epidemic, affecting as many as one-third of adults in the United States. That’s up to 83.6 million people routinely getting less than 7 hours of sleep per night. And women are twice as likely as men to have difficulties falling asleep or staying asleep, according to the National Sleep Foundation.
Sleep is important to our well-being because that’s when our bodies recharge and release hormones like cortisol and human growth hormone that repair tissues and mend muscles. A good sleep routine helps our brains recuperate and process all the memories and thoughts of the day. It’s just as important to our overall health as a nutritious diet and regular exercise. On the flip side, ongoing sleep deprivation can compromise our cardiovascular and neurological systems, which can lead to chronic illnesses such as cancer, diabetes, depression, high blood pressure and obesity, according to the CDC. A recent study done at the University of California, San Francisco, found that people who sleep 5 hours or less each night were 17 percent more likely to catch a cold and 51 percent more likely to get the flu or pneumonia than people who sleep 7 hours or more.
In the age of Snapchat, Facebook, Pokemon Go, and the non-stop workweek, our urge to remain always on often overwhelm our physical need to get adequate rest and sleep. “Left alone, our circadian rhythm would determine when we are awake, when we eat, when we are alert, and when we are active,” says Dr. Debra DeLuca, a sleep medicine specialist and medical director of quality at the Capital Health Center for Sleep Medicine. “This rhythm is largely determined by the day-night cycle, and it changes over time, with people going to bed and waking up earlier as they get older.”
The National Sleep Foundation recently established guidelines for how much sleep we should get per night based on age, from newborn to elderly. Dr. DeLuca points to a range of factors that can cause our internal clock to get out of sync, from stress to illness to jet lag. But, she adds, one night of inadequate sleep isn’t going to kill you since you can recover from short-term sleep deficits by getting a full night of sleep during the next one or by taking a brief nap that isn’t too close to (meaning at least 12 hours before) your bedtime. But going too long without a decent night’s sleep will eventually build up a sleep deficit that can impact your physical and psychological health.
“Some people’s internal clocks can also have them falling asleep later than the average person,” says Dr. Marcella Frank, medical director of the Capital Health Center for Sleep Medicine. “Part of the increased use of sleeping pills and melatonin comes from people who are trying to shift their internal clocks to make their sleep patterns more compatible with their lives.”
Instead of medication, Dr. DeLuca recommends waking up at roughly the same time every day no matter how bad your night of sleep was. “If you establish a regular wake up time, your body will adjust to it, but not if you sleep in on weekends and have long naps,” she says. “Just establish a set bedtime ritual, such as a warm bath, listening to calm music or reading a book, and follow the same routine, at the same time, each night.” A regular routine is key to maintaining a healthy sleep cycle that gives your body all the rest it needs without interruption.
A Healthy Dose of Shut-Eye
The National Sleep Foundation, recently issued new recommendations on how much sleep we should all be getting each day. They are divided into nine age categories and based on a review of research and a consensus from a group of 18 experts in sleep, physiology, science, and medicine:
- Newborns (0 to 3 months) – 14 to 17 hours
- Infants (4 to 11 months) – 12 to 15 hours
- Toddlers (1 to 2 years old) – 11 to 14 hours
- Preschoolers (3 to 5 years old) – 11 to 14 hours
- School age (6 to 13 years old) – 9 to 11 hours
- Teens (14 to 17 years old) – 8 to 10 hours
- Young adults (18 to 25 years) – 7 to 9 hours
- Adults (26 to 64 years old) – 7 to 9 hours
- Older adults (65 and older) – 7 to 8 hours

An estimated 25 percent of people over the age of 65 have some degree of sleep apnea.
Sleep Aids
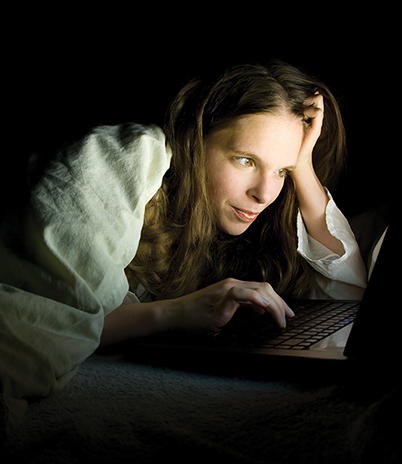
If you’re looking to become a better sleeper, here are a few products that can help. They each work by limiting the amount of light around you during bedtime. “Your brain interprets light as a signal to be alert,” says Dr. DeLuca. “And blue light, like the kind emitted by your phone and computer screen, tells your body to stop producing melatonin, the hormone that makes you feel sleepy.”
 Drift Light
Drift Light
An LED light that casts a warm hue and gradually dims over a period of 37 minutes, which is about how long it takes the sun to set. ($25, drift-light.com)
F.lux
A program for your laptop that adjusts your screen’s light based on the time of day, providing warmer hues in the evening that don’t mess with your internal clock.
Night Shift
A feature built into iPhones and iPads that shifts the hue of a device’s backlight to limit your exposure to blue light near bedtime. Apple is expanding on this feature by adding a bedtime function to the next version of its iPhone operating system that prompts you when to go to sleep so you can get a full night’s rest.
A history of restless rest
While anyone can hit a rough patch when it comes to sleep, they’re often just bleary-eyed glimpses into the unending cycle of restless nights that someone with a serious sleep disorder experiences on a regular basis. Up to 70 million adults in the United States suffer from a sleep disorder with over half failing to get proper diagnosis or treatment, according to research published in the journal Sleep Medicine.
“There are 85 different sleep disorders,” says Dr. Frank. “Some can be diagnosed from a sleep study and some are diagnosed clinically.” She notes that most of the patients treated at the Capital Health Center for Sleep Medicine suffer from snoring, sleep apnea, and insomnia, but the Center also sees a fair amount of dream-enacting behavior, sleep walking, sleep talking, and restless legs syndrome. Every one of these disorders can derail your life—impacting your job performance, your relationships, and your sense of well-being.
That’s also why the sleep studies conducted at the Capital Health Center for Sleep Medicine are so comprehensive, involving a wide range of sensors that record in minute detail what your body does during sleep. “Sleep studies allow us to figure out exactly what’s waking a patient up and zero in on the issues that need to be addressed,” says Dr. Frank. “So, the major things we look at—breathing, oxygen levels, brain activity during sleep, and leg movement—capture that.” To experience what goes into a sleep study first hand, I drop by the center one night for a sleepover.
Going through a sleep study is like checking into a hotel, but with a few extra wires and sensors (28 to be exact). Before getting into bed, a technologist attaches sensors and wires to my scalp, chest, face, and legs, as well as belts around chest and abdomen to monitor the effort that goes into my breathing. Then, after I put my head on the pillow, the sleep technologist connects the last one under my nose—a breath sensor that records airflow pressure and temperature, as well as exhaled carbon dioxide. The other end of the wires connect to a machine that records everything. “All this information used to be recorded on paper, and a single night took up a thousand pages,” says Dr. Frank.
“Brain wave activity indicates whether a patient is asleep or awake and, along with heart rate, eye movement, and chin muscle activity, show what stage of sleep a patient is in,” she says.
How much deep, light, and REM sleep you get each night as well as how you cycle through each stage are important indicators of your sleep health. In general, a full sleep cycle takes about 90 minutes to complete, which means the average person rotates through several cycles between dusk and dawn, and they generally spend most of the first half of the night in deep sleep and most of the second half in REM sleep.
“As people get older, everything gets floppy and sags, which can compromise breathing,” says Dr. Frank. “This can lead to apnea and severe snoring, which can both disrupt a person’s sleep cycles and cause fragmented sleep.” Sleep apnea happens because the throat collapses during sleep, she says, forcing your brain to choose breathing properly over staying asleep. The American Sleep Apnea Association estimates that 90 million people snore and more than 18 million people have some degree of sleep apnea, though that number could be higher because most people often don’t realize they have it. “When left unchecked, the condition increases your risk of high blood pressure, diabetes, heart attacks, strokes, and coronary artery disease.”
“Most people who have sleep apnea are overweight,” says Dr. Frank. “They generally gain weight as they get older, and as they get heavier the risk of sleep apnea gets worse.” Slimming down helps most sleep apnea sufferers breathe easier because it reduces the flabby obstructions along the sides of the throat and underneath the diaphragm. Age is also a factor: “An estimated 25 percent of people over the age of 65 have some degree of sleep apnea.”
Along with the sleep study, an evaluation by an ear, nose, and throat doctor will look for structural blockages in the nose, the sinuses, the septum, and the back of the throat. “If after all this someone is diagnosed with sleep apnea, then they’ll often come back to the Center to try out a CPAP machine for a night,” says Dr. Frank. CPAP stands for continuous positive airway pressure, and it holds the throat open to allow an apnea sufferer to breath naturally. An overnight CPAP trial allows the patient and technologists to get the pressure right and the mask comfortable enough to sleep in.
Rest Assured
“What many of us lack is a wind-down period that would let our brain know it is time for rest,” says Dr. DeLuca. “This often means unplugging—both figuratively and literally—from work and mobile devices that keep us on our toes all day.” Here’s what she recommends for a healthy diet of golden slumbers:
- Make your bedroom the place for sleep and sex—no other activities
- Keep your bedroom quiet, dark, and cool for sleep
- No nightcaps before bed—it takes the body 4 hours to process alcohol
- Exercise is good for sleep but not when you do it too close to your bedtime
- Going to bed with a full stomach can cause your sleep to be fitful
- Reduce or eliminate caffeine and nicotine intake in the hours leading up to bedtime
- If you nap during the day, try to do it at least 12 hours before your bedtime
- If you’re lying in bed for more than 20 minutes, get up and do something else, then get back in bed and repeat your routine
Sleeping awake
While my sleep issues are annoying, they aren’t chronic. Sure, I’m laying awake in the middle of the night for the second time this week, but that happens to plenty of people fighting through stress. If I just relax, I’m sure I’ll fade off any minute. “Insomnia can be triggered by a number of different things including apnea and affects about 10 to 15 percent of adults,” says Dr. DeLuca.
According to the National Sleep Foundation, chronic insomnia is associated with stress, anxiety, and depression and is defined as having trouble falling or staying asleep at least three times per week for 3 months or longer. “There are many different factors—environmental, psychological, and physical—that go into insomnia,” says Dr. Frank. “So we do a long assessment and ask a lot of questions to figure it out.”
While middle-of-the-night insomnia is more common than onset insomnia (trouble getting to sleep), both are complicated by stress, depression, and anxiety. Oftentimes the prospect of not sleeping intensifies the agitated feelings that were keeping you awake in the first place, making you even more anxious. This is how anxiety and insomnia can create a self-perpetuating cycle that often needs to be addressed through treatment.
“When it comes to insomnia, sleeping pills are just band-aids on what is often a more serious problem,” says Dr. Frank. “People can get addicted and build a tolerance to sleeping pills. When people come here, our goal is to find the cause and fix it.” There are cognitive and mind-body techniques that help people with anxiety settle into sleep, and overall healthy sleep practices that can improve sleep for many people with chronic insomnia.
After staring at the ceiling for another 15 minutes, I finally drift off to sleep. And that’s a good thing because my Real Woman article isn’t going to write itself.





